What is heart failure?
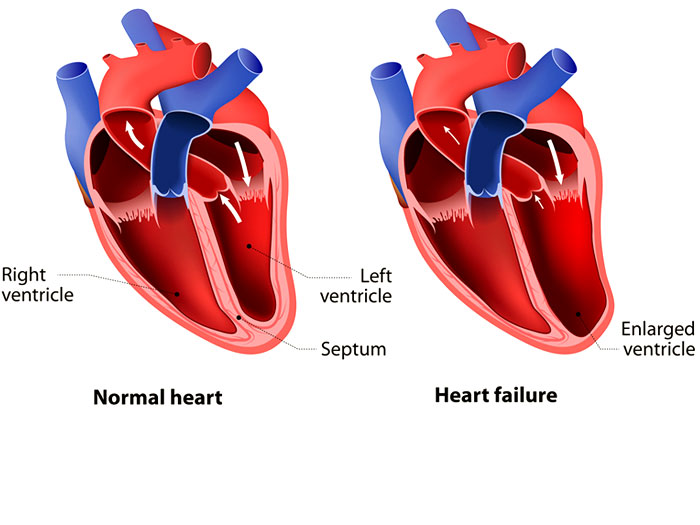
Heart failure is a condition in which the heart is not is not able to pump enough blood as it should. This leads to reduced blood supply to all the organs of the body. The pumping power is reduced ( reduced ejection fraction ) in heart failure. But heart failure can also occur with preserved pumping power ( heart failure with preserved ejection fraction )
What are the types of heart failure?
Types of heart failure:
Heart failure could occur due to failure of right side of heart or left side of heart. Sometimes, both sides of heart might be affected.
- Left-sided heart failure: in left heart failure, the fluid may get collected in lungs causing shortness of breath.
- Right-sided heart failure: in right heart failure , fluid might get collected in abdomen, legs and feet, causing swelling.
Heart failure with preserved ejection fraction is the condition in which the heart can't relax and there is problem with the filling of the heart.
Risk Factors
What are the risk factors for heart failure?
Some factors are related to your lifestyle habits which can be modified and few are non-modifiable risks.
Age: Older people have a higher risk of heart failure because aging can weaken and /or stiffen your heart.
Family history and genetics. Heart failure can run in family. You have a higher risk of heart failure if people in your family have been diagnosed with heart failure at early age.
Lifestyle: An unhealthy diet, smoking, heavy alcohol use can raise your risk of heart failure.
Other medical Illness . lung disease, infection mostly viral SARS-CoV-2 may raise your risk of heart failure. Long-term health conditions such as obesity, high blood pressure, diabetes, anemia thyroid disease, or iron overload also raise your risk.
Medicines: Many of the medicines used for treatment of cancer chemotherapy can affect your heart muscles making them weak
Race or ethnicity
Sex. Heart failure is common in both men and women.
Causes
Causes of heart failure :
- Coronary artery disease. Blockages in the heart arteries may limit your heart's supply of blood, resulting in weakening of the heart muscle.
- Heart attack. A heart attack is a form of sudden blockage of the blood supply to the heart muscles cause the heart muscles to go weak.
- Heart valve disease. Patients with untreated heart valve problems are at higher risk of heart failure
- High blood pressure. Makes your heart work harder causing it to weaken over a period of time.
- Irregular heartbeats. Irregular heart beats or non –synchronous heart rate and rhythm causes heart failure
- Heart defects present since birth : Some might have structural/ functional heart defects since birth. If un treated at right time, could lead to heart failure.
- Diabetes. Diabetes is know to cause early aging of blood vessels.
- Certain other medications. Some medications are known to cause heart failure in some.
- Alcohol use. Drinking too much alcohol could lead to heart failure.
- Obesity. People who have obesity have a higher risk of developing heart failure as the body has to pump blood adequate to support a big body.
- Viruses. Certain viral infections can cause damage to the heart muscle. Viral myocarditis is a known cause in children.
Myocarditis is very common in children. Myocarditis could be classified into infectious and non-infectious myocarditis.
The following pathogens are known causes of infectious myocarditis:
- Viruses: adenovirus, influenza, hepatitis B, hepatitis C, parvovirus, herpes simplex virus, echoviruses, coxsackievirus, Epstein-Barr virus (EBV), rubella, human immunodeficiency virus and coronaviruses, including SARS-CoV-2
- Bacteria: staphylococcus, streptococcus, Corynebacterium diphtheriae and Borrelia burgdorferi, the bacteria the causes Lyme disease
- parasites: including Trypanosoma cruzi and Toxoplasma gondii
- Fungi: Candida, Aspergillus and Cryptococcus genera
Causes of non infectious myocarditis in children include medications, including some medicines given for chemotherapy ; chemical exposure; radiation or medical conditions, like lupus, Wegener’s granulomatosis, sarcoidosis , etc.
Symptoms
What are the symptoms?
- Shortness of breath (also called dyspnea)
Initially the shortness of breath could be only at strenuous activity. As the disease progresses, the shortness of breath might worsen as restrict the activity to just going to the bath room. It could also worsen to cause breathlessness even on sitting. - Persistent coughing or wheezing
- Buildup of excess fluid in body tissues (edema): Selling on feet, face and on abdomen could occur due to excess accumulation of fluid in the body.
- Tiredness, fatigue: it occurs due to reduced blood supply to the body organs
- Lack of appetite, nausea
- Confusion, impaired thinking: it might occur if there is reduced supply of blood to the brain.
- Increased heart rate: some might notice very fast heat beats or palpitations.
Stages
ACC/AHA Stage Symptoms
- At high risk for heart failure but without structural heart disease or symptoms of heart failure.
- Structural heart disease but without signs or symptoms of heart failure.
- Structural heart disease with prior or current symptoms of heart failure.
- Refractory heart failure requiring specialized interventions.
Treatment
Treatments for Each Stage of Heart Failure:
Identification of heart failure at an early stage is most crucial for the success of treatment. Diagnosis at right time could slow down the progress of heart failure.
Treatment depending on the stage :
Stage A:
(At high risk for heart failure)
- Quit smoking.
- Exercise regularly
- Treat high blood pressure
- Treat lipid disorders
- Discontinue alcohol or illegal drug use
If you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions, taking medications as prescribed
Stage B:
(Heart disease, without signs of heart failure)
All patients should take medicines to improve pumping power of the heart Surgery options should be discussed for coronary artery or valve disease.
Stage C:
(Heart disease, with signs of heart failure)
- Diuretics (water pills) to get rid of excess water may be prescribed if symptoms persist
- Restrict dietary sodium (salt)
- Monitor weight
- Restrict fluids (as appropriate)
- Pacemaker or ICD may be recommended
Stage D:
(Heart failure not responding to treatments)
Patient should be evaluated to determine if the following treatments are available options:
- Heart transplant
- Ventricular assist devices
- Surgery options
- Continuous infusion of drugs to keep heart pumping
