What is lung transplant?
A lung transplant is a surgical procedure to replace a diseased or failing lung with a healthy lung, usually from a deceased donor ( brain dead ). A lung transplant is reserved for people who have tried medications or other treatments, but their condition hasn't sufficiently improved.
Depending on your medical condition, a lung transplant may involve replacing one or both of the lungs. In some situations, the lungs may be transplanted along with a donor heart.
While a lung transplant is a major operation that can involve many complications, it can greatly improve your health and quality of life.
When faced with a decision about having a lung transplant, know what to expect of the lung transplant process, the surgery itself, potential risks and follow-up care.
Why it's done
Unhealthy or damaged lungs can make it difficult for your body to get the oxygen it needs to survive. A variety of diseases and conditions can damage your lungs and keep them from functioning effectively. Some of the more common causes include:
Diffuse Parenchymal Lung Disease including:
- Idiopathic pulmonary fibrosis (UIP and NSIP)
- Lung fibrosis in association with connective tissue disease
- Occupational lung fibrosis
- Drug / toxic lung fibrosis
- Chronic hypersensitivity pneumonitis
- Sarcoidosis
- Lymphangioleiomyomatosis
- Langerhan’s cell histiocytosis
Diffuse Parenchymal Lung Disease including:
- Smoking related chronic obstructive pulmonary disease (COPD)
- Alpha 1 antitrypsin deficiency
- Obliterative bronchiolitis
- Chronic asthma
Pulmonary vascular disease including:
- Idiopathic pulmonary arterial hypertension
- Pulmonary arterial hypertension associated with connective tissue disease
- Complex congenital heart disease with Eisenmenger’s syndrome
- Chronic thromboembolic pulmonary hypertension unsuitable for or unresponsive to pulmonary thrombo endarterectomy
- Pulmonary veno-occlusive disease
- Pulmonary capillary haemangiomatosis
Suppurative lung disease including:
- Cystic Fibrosis (CF)
- Non-CF bronchiectasis
COVID induced lung dysfunction
Lung damage can often be treated with medication or with special breathing devices. But when these measures no longer help or your lung function becomes life-threatening, your health doctor might suggest a single-lung transplant or a double-lung transplant.
In some cases, people with serious heart and lung conditions may need a combined heart-lung transplant.
What You Can Expect
The procedure will be done with general anesthesia, so you will be unaware and won't feel any pain. You'll have a tube guided through your mouth and into your windpipe so that you can breathe.
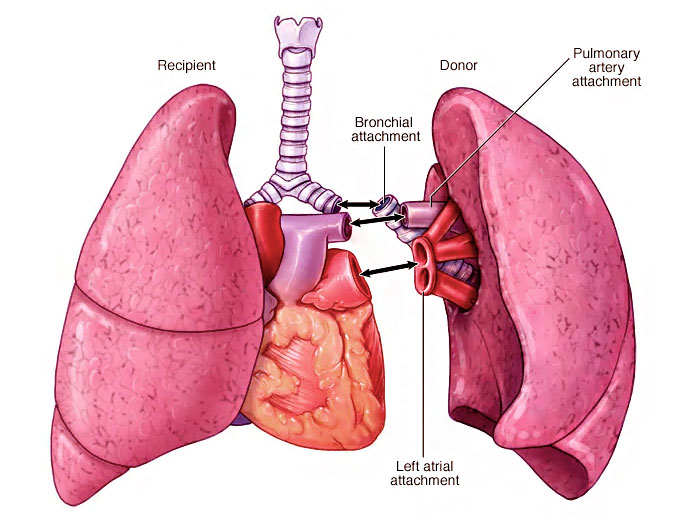
Your surgeon will make a cut in your chest to remove your damaged lung. The main airway to that lung and the blood vessels between that lung and your heart will then be connected to the donor lung. For some lung transplants, you may be connected to a heart-lung bypass machine, which circulates your blood during the procedure.
Immediately after the surgery, you'll spend several days in the hospital's intensive care unit (ICU). A mechanical ventilator will help you breathe for a few days, and tubes in your chest will drain fluids from around your lungs and heart.
As your condition improves, you'll no longer need the mechanical ventilator, and you'll be moved out of the ICU. Recovery often involves a one- to three-week hospital stay. The amount of time you'll spend in the ICU and in the hospital can vary.
What happens after lung transplant
After you leave the hospital, you'll require about three months of frequent monitoring by the lung transplant team to prevent, detect and treat complications and to assess your lung function. During this time, you'll generally need to stay close to the transplant center. Afterward, the follow-up visits are usually less frequent, and you can travel back and forth for follow-up visits.
Your follow-up visits may involve laboratory tests, chest X-rays, an electrocardiogram (ECG), lung function tests, a lung biopsy and checkups with a specialist.
What is lung biopsy?
In a lung biopsy, your health care provider removes very small lung tissue samples to test for signs of rejection and infection. This test may be conducted during a bronchoscopy, in which the provider inserts a small, flexible tube (bronchoscope) through the mouth or nose into the lungs. A light and a small camera attached to the bronchoscope allow the provider to look inside the lungs' airways. The provider may also use special tools to remove small samples of lung tissue to test in a lab.
Your transplant team will monitor you closely and help you manage immunosuppressant medications and its side effects. Your transplant team may also monitor and treat infections. Your doctor might prescribe antibiotic, antiviral or antifungal medications to help prevent infections. Your transplant team may also instruct you about ways you can help prevent infections at home.
What happens after lung transplant:
You'll be monitored for any signs or symptoms of rejection. These can include:
- Shortness of breath
- Fever
- Coughing
- Chest congestion
- It's important to let your transplant team know if you notice any signs or symptoms of rejection.
You'll generally need to make long-term adjustments after your lung transplant, including:
Taking immunosuppressants. You'll need to take immunosuppressant medications for life to suppress your immune system and prevent rejection of the donor lung or lungs.
Managing medications, therapies and a lifelong care plan. Your health care provider may give you instructions to follow after your transplant. It's important to take all your medications as your provider instructs. It's also important to check your lung function at home as directed by your provider. Attend follow-up appointments and follow a lifelong care plan.
Living a healthy lifestyle. Living a healthy lifestyle is key in helping to keep your new lung healthy. Your health care provider may advise you to not use tobacco products and to limit alcohol use. Following a nutritious diet also can help you stay healthy.
Exercise is an extremely important part of rehabilitation after your lung transplant and will begin within days of your surgery. Your health care team works with you to design an exercise program that's right for you
Talk to your health care provider if you're feeling stressed or overwhelmed.
How are the results after lung transplant?
A lung transplant can substantially improve your quality of life. The first year after the transplant — when surgical complications, rejection and infection pose the greatest threats — is the most critical period.
Some people have lived 10 years or more after a lung transplant. Data suggests that about 60 % of patients would be alive at 5 years of transplant.
What are the advantages of lung transplant ?
Main advantages of a successful lung transplant:
- Most lung transplant patients live longer
- Most patients enjoy a better quality of life
What are the risks/ complications?
A lung transplant requires complex surgery and can cause problems for some patients.
Main complications of a lung transplant:
- operation is associated with risks like bleeding, infections
- You may need further surgery to fix any problems
- Though rare, it is possible that the transplanted lung doesn’t work ( primary graft dysfunction )
- There is a risk of dying after this major operation
- Several nerves around the area of the lung transplant may be damaged. Nerves to vocal cords, breathing muscle, food pipe are more prone to be injured. Discuss with your doctor for details
- New onset or worsening of diabetes
- Stroke, or clots in arteries or veins.
- Very rarely could have heart problem / tummy problem after lung transplant.
- The chances of you getting cancer in new lungs is rare as the lungs are screened before transplant. But still there is a remote possibility of you getting cancer after transplant.
What is primary graft dysfunction ?
The new lungs might not start functioning immediately. This is called primary graft dysfunction.
If the new lungs are not working after the transplant, you will require breathing support. This is either through mechanical ventilation or need external heart lung support called Extra Corporeal Membrane Oxygenation (ECMO).
Important Links: Best Heart Surgeon in Prabhadevi | Best Bypass Surgeon In Prabhadevi | Best Cardiologist In Prabhadevi | Best Tavi in Prabhadevi | Best Angioplasty in Prabhadevi | Best Transplant Doctor in Prabhadevi
